This page is designed to help you understand the most recent eligibility and enrollment criteria for selling D-SNPs. Once you’ve verified your client’s D-SNP eligibility (See the Dual Special Needs Plans page) you are then able to enroll the client into a UnitedHealthcare D-SNP following the appropriate enrollment period. The table below outlines the times when you can enroll eligible clients into a D-SNP.
| Selling Circumstance | Time | Selling Restrictions |
|---|---|---|
| AEP | October 15 – December 7 | None, except for one plan in New Mexico and Hawaii, which each require Full Dual eligible members to enroll in UHC Medicaid first. |
| Medicare Advantage Open Enrollment Period (OEP) |
January 1 – March 31 | Consumers who have Medicare Advantage can switch to another Medicare Advantage plan with or without drug coverage. |
| Integrated Care SEP | Year-Round | Yes, state-dependent. See the state At-A-Glance documents. |
Special Circumstances SEP |
Year-Round |
Click here for more information |
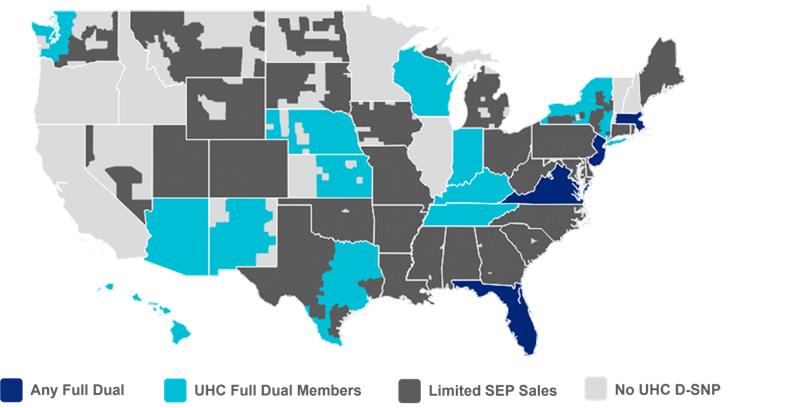
One key area to highlight is the new Special Election Period (SEP) for Dual Eligible members called the Integrated Care SEP. The new Integrated Care SEP allows a once-per-month election for Full Dual eligibles (QMB+, SLMB+, FBDE) to enroll into a Fully Integrated Dual Eligible (FIDE), Highly Integrated Dual Eligible (HIDE) or an Aligned Integrated Plan (AIP) Special Needs Plan (SNP). View the Medicaid Categories of Eligibility (COE) Guide to learn more about Full, QMB and Partial categories and how they are classified.
| D-SNP Eligibility | Scenario | Market |
|---|---|---|
| Any Full Dual |
|
AZ (FIDE), DC, FL (HIDE), MA, NJ, VA |
| Full Duals with UnitedHealthcare Medicaid |
|
AZ (HIDE), FL (FIDE), HI, IN, KS, KY, NE, NM, NY, TN (FIDE), TX, WA, WI |
Limited to special |
|
AL, AR, CO, CT, DE, GA, IA, LA, MD, ME, MI, MO, MS, MT, NC, ND, NV, OH, OK, PA, RI, SC, SD, UT, WV, WY |